Third Party Administrators Use Intelligent Capture Technology for a Happier Customer
New technologies introduce new customer expectations, and now more than ever, the speed of artificial intelligence has increased the rate at which customers desire to be serviced, particularly among patients and payers. Service Level Agreements (SLAs) need to be met, and automation is the key.
Third Party Administrators (TPAs) that find themselves with a backlog of health insurance claims can make their lives easier with the latest advancements in intelligent capture technology and optical character recognition. We call this advancement, Intelligent Document Processing.
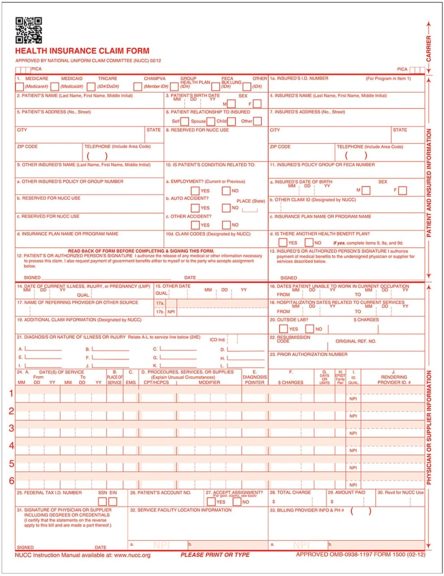
Capture Your CMS Forms
Fueled by intelligent document processing, our AI-enabled capture technology can read claims data on CMS forms. It focuses on both header and footer data, as well as the determined body data you need it to read. Once the data has been captured, we can put it into a workflow, integrated with your claims system, so the data can be sent to the right people for processing. The workflow can also help an insurer to find fraud, deny claims, and ask healthcare staff for supporting information decreasing denials and fees.
Automate What You’re Doing Manually
Free your staff who is manually keying HICF information into your claims tool to do more valuable work. We can provide a consult with examples from some of our customers who are using this service.
Contact us today to start the conversation!
We can help you decide pretty quickly whether intelligent data capture would be a good fit for your insurance agency. With nearly three decades of experience in automation, we just need about 5 minutes of Q&A.




